Author: John Hilinski, CoAuthors: Anil R. Shah & Kris S Moe
Nasal tip surgery is among the most complex and difficult tasks in rhinoplasty surgery. Vertical dome division (VDD) is one of a variety of techniques that may be used in refining nasal tip appearance. Collectively, vertical dome division (VDD) refers to one of many methods of vertically dividing the lower alar cartilage at or near the dome to modify nasal tip aesthetics. The technique was originally recommended as an alternative in altering tip projection and appearance while minimizing use of implants and the degree of postoperative tip ptosis. Vertical dome division (VDD) targets various nasal deformities, including overprojection or underprojection, suboptimal rotation, disproportionate lobule ratios, and broad or asymmetric tip. The surgeon must strive to achieve an aesthetically pleasing nasal tip that is in balance with the remainder of the nose without compromising nasal airway function.
The typical patient presenting for vertical dome division (VDD) usually
has a poorly defined or malpositioned tip with a combination of
abnormal projection/rotation, broad or amorphous lobule, asymmetric tip
defining points, and/or boxy, trapezoidal base.
Adherents to this principle argue that horizontal excisional techniques
rely too heavily on unpredictable and uncontrollable postoperative
scarring to produce desired tip results. Proponents of vertical dome
division (VDD) believe that vertical incisional and excisional
techniques, on the other hand, offer a more definitive and reliable
means to achieve desired tip changes.
In principle, the technique of vertical dome division (VDD) separates the medial and lateral crura into 2 independent units. By transecting the dome, the inherent spring within the arch is released and allows realignment of the newly divided medial and lateral segments to reconstruct the nasal tip.
Vertical dome division (VDD) is typically reserved for more complicated
cases that require greater changes to effect tip refinement than could
be achieved using other techniques. Nearly all variations of vertical
dome division (VDD) used today involve some modification of the original
Goldman technique
The lobule is defined as the portion of the nasal tip complex that is situated anterior to the nostrils; it extends from the tip defining point to the junction with the columella, as observed on base view. The alar cartilage (lower lateral cartilage) is C-shaped and can be divided into the medial, middle, and lateral crus. The middle (intermediate) crus comprises the domal segment and largely influences the shape of the lobule and, therefore, the form and definition of the nasal tip. The dome is considered the highest arching segment within the nasal vestibule.
The lobule size can be assessed in comparison to the columellar length. If the base view demonstrates a columellar-to-lobule ratio of approximately 2:1, the structural support and configuration of the nasal tip is considered adequate. A long nasal length reflects an acute nasolabial angle; a short length reflects an obtuse nasolabial angle.
The anatomy of the nasal tip is often described using the tripod concept to facilitate understanding of the key structural components and to provide a simple explanation of tip dynamics. According to this analogy, the cartilaginous framework of the lower third of the nose is compared to a tripod that is attached to the facial frontal plane. The 2 individual lateral crura represent 2 legs of the tripod, and the conjoined medial crura and caudal septal attachments correspond to the third leg.
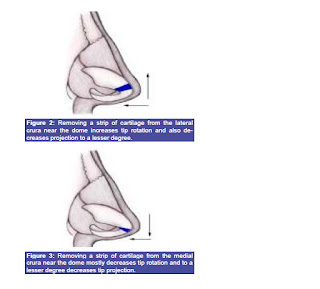
By lengthening or shortening any or all legs of the tripod, the changes that will be effected in tip projection and rotation can be predicted. For instance, techniques that augment or lengthen the medial crural segment enhance projection. Shortening the medial crura or disrupting their septal attachments without reduction of lateral crural length decreases projection and rotation of the nasal tip. Shortening the lateral crura and maintaining or lengthening the medial crural segment would be expected to increase rotation.
Contraindications
Vertical
dome division (VDD) is predominantly contraindicated in patients with
relatively thin skin. These patients are particularly prone to
developing visible cartilage edges along the nasal tip region. This
results from contraction of the thin overlying skin and soft tissue
envelope around the new and more prominent medial cartilaginous strut. A
thick overlying skin and soft tissue envelope is better able to cushion
the appearance of prominent cartilaginous structures, such as those in
vertical dome division (VDD).
Avoid classic vertical dome division (VDD) in patients who show evidence of already weakened lateral nasal walls. Dividing the domal region without reapproximation of the cartilage segments disrupts the integrity and continuity of the lower lateral cartilage. The lateral nasal wall is more susceptible to structural collapse than the newly reinforced medial footplates. As a result, lateral wall weakening and collapse are further potentiated.
The original technique is highly focused on manipulation and repositioning of only the medial crura, with no attempt made to reconstruct the remaining lateral crural segment and alar rim. Postoperatively, the medial crura and columella are sufficiently stable to resist loss of projection. Some loss of lateral support, which could result in lateral wall collapse and alar retraction, may occur. Vertical dome division (VDD) is also associated with bossae formation. This is most frequently seen in patients with thin skin and firm cartilages. Disruption of the underlying vestibular mucosa and skin, such as in the Goldman technique, also predisposes the patient to possible stenosis.
Avoid classic vertical dome division (VDD) in patients who show evidence of already weakened lateral nasal walls. Dividing the domal region without reapproximation of the cartilage segments disrupts the integrity and continuity of the lower lateral cartilage. The lateral nasal wall is more susceptible to structural collapse than the newly reinforced medial footplates. As a result, lateral wall weakening and collapse are further potentiated.
The original technique is highly focused on manipulation and repositioning of only the medial crura, with no attempt made to reconstruct the remaining lateral crural segment and alar rim. Postoperatively, the medial crura and columella are sufficiently stable to resist loss of projection. Some loss of lateral support, which could result in lateral wall collapse and alar retraction, may occur. Vertical dome division (VDD) is also associated with bossae formation. This is most frequently seen in patients with thin skin and firm cartilages. Disruption of the underlying vestibular mucosa and skin, such as in the Goldman technique, also predisposes the patient to possible stenosis.
With use of newer modified techniques (Hockey stick excision, Lipsett, Simons, Adamson, and others) and caution, vertical dome
division (VDD) can be used successfully in nasal tip refinement with
limited postoperative complications and reliable long-term results.
Most practitioners using vertical dome division (VDD) today perform some modification of the original Goldman tip procedure.
Adamson reported that approximately 5% of patients required revision
surgery for postoperative tip abnormalities and irregularities
attributed to use of vertical dome division (VDD).[10] These
abnormalities were primarily nasal bossae and lobule asymmetries.
Abnormalities were nearly 3 times as likely to occur in revision cases
as in primary rhinoplasty; incidence was lower with use of the incision
and overlap method.
Vertical dome division (VDD) is likely to remain controversial in the future. As knowledge of nasal tip surgery evolves, so too will further modifications of our existing tip techniques to attain more predictable outcomes.
http://emedicine.medscape.com/article/841313-overview
The Endonasal Approach to Rhinoplasty
Robert L. Simons and Lisa D. Grunebaum Ch.68 Rhinology and Facial Plastic Surgery
Today's trends in nasal tip surgeries are for improved visualization with preservation of the cartilage as well as better medial stabilization and support. These tenets are inherent in vertical dome division techniques. It is important to remember that VDD is an incisional technique that allows for repositioning of the nasal tissue and should not be combined with excisional techniques. One should always leave behind more than one takes. Preservation of at least 6-8mm of lateral crus will help prevent alar collapse and help stabilize the nasal base as well as allow for a strong natural-appearing tip.VDD allows for narrowing, rotation, and change in tip projection by repositioning rather than excision of any sizable amount of cartilage.
The Effectiveness of modified VDD Technique in reducing nasal tip projection in rhinoplasty
B.Gandomi, M.H. Arzaghi, M. Rafatbakhsh
Our technique involves the overlapping of the incised edges of the medial and lateral segments, and suture approximation to restore the integrity of the alar cartilage. The technique allows a more stable configuration for the maintenance of nasal tip support. The overlapping and reapproximation of the medial and lateral units ensure the long-term stability of the newly reconstructed nasal tip complex, and reduce the tendency towards postoperative cartilaginous abnormalities that may accompany scar fibrosis and contracture.